In 2020 NHS Somerset introduced an innovative, patient centred Covid Recovery Service last December, designed to support patients across the county suffering from the effects of Long COVID. This service was part of an initiative by NHS England, funding 69 clinics across the country. There is growing evidence, that shows a number of people suffering from COVID-19, will go on to struggle with the effects of Long COVID, (a term used to describe those people who continue to experience symptoms such as breathlessness, chronic fatigue, brain fog, anxiety and stress) three months or more after having initially falling ill.
The symptoms of long COVID are wide-ranging and fluctuating. However, many patients recover with support, rest, symptomatic treatment, and with a gradual increase in physical activity.
While we have learned lots about Covid-19, we still need to learn more about its long-term effects, which we know can be debilitating, even for young, fit people, or those who did not go to hospital.
The Somerset Covid Recovery Service will not only give us an opportunity to support patients with symptoms associated with Long COVID, but will also help us learn out more about Long COVID and find new ways to help people affected by it.
Currently the Somerset COVID Recovery Service is only available through GP referral. It is important that anyone experiencing symptoms of COVID-19 for more than 12 weeks speak to their GP about their COVID recovery, who will, as part of this conversation be able to review a patient’s clinical needs. The multi-disciplinary Covid Recovery Service for patients with Long Covid symptoms, runs in our primary care service, as a virtual clinic. Patients can be referred into the service via their local GP.
It will work alongside other health teams to develop a support plan that will help improve patient’s health outcomes and quality of life.
Rachael Rowe, Head of Long Term Conditions at NHS Somerset says “We know it is vital that people with Long COVID get the support they need. Our Covid Recovery Service enables us to draw on specialist services across Somerset such as mental health and physio support, in a co-ordinated manner to address a patients individual needs, ensuring they can benefit from a wide range of specialist advice and support.”
Advice and support
Although there is no single treatment that cures symptoms associated with Long Covid, there is lots of advice on the Covid Recovery app for self-care that patients can take to help with their recovery ‘Your COVID Recovery | Supporting your recovery after COVID-19”
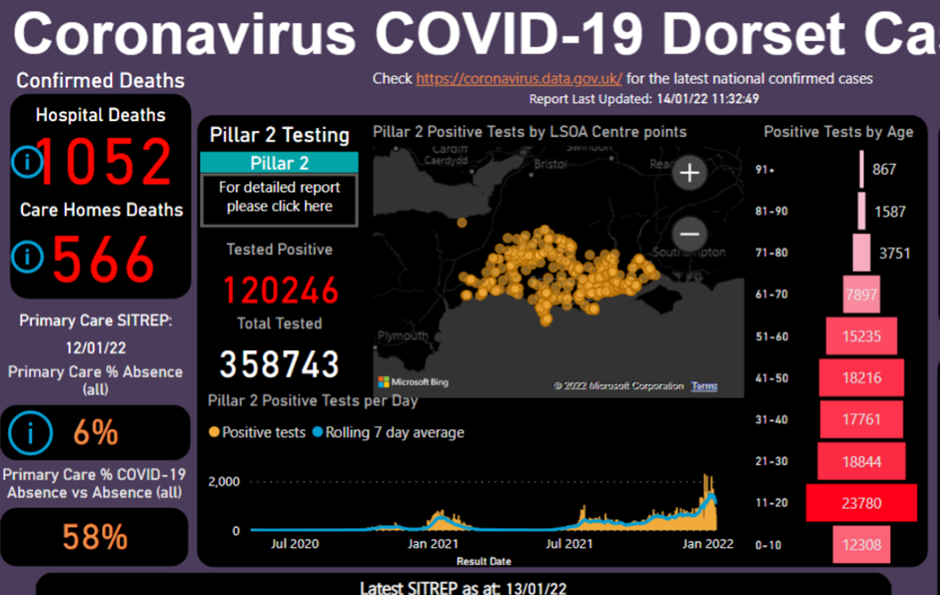
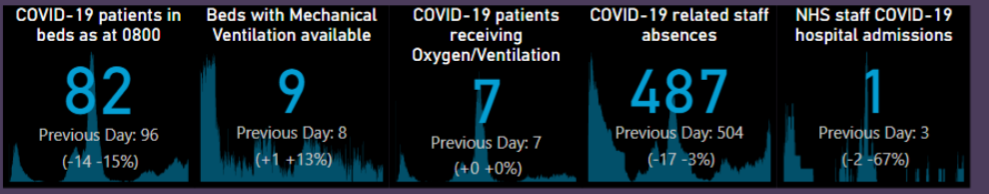
DiiS supports the COVID-19 response through an automated, live data system–wide view of COVID cases, across acute, community and primary care settings, enabling us to better understand the spread of the disease locally and model capacity and demand. Analytics focusing on vulnerable or at risk populations, including those with mental health conditions, has helped clinical colleagues to identify specific groups who may benefit from a directed, pro-active approach. Using this data they have focused their workforce on these groups dependent on social as well as clinical need.
Demographic markers such as gender and ethnicity have been added into DiiS tools to support Dorset’s response to the COVID pandemic.
This has highlighted the health inequalities experienced throughout the pandemic. The analytics are interactive and filterable by a number of metrics including deprivation, such as most and least 20% deprived, as well as other vulnerabilities including risk of social isolation, unhealthy behaviours and active safeguarding flags.
A live view of our flu vaccination status is informing the winter flu campaign informing comms strategies as well as helping clinicians to target hard to reach populations.
“Clinicians are delighted that the data doesn’t give you answers. It helps you refine your questions.
The amount of effort people gave to responding to those
questions … “I’ve seen that happen in the past, but not at this scale.”
In July 2020 we held our first online event; “An intelligent response to COVID through data-driven health systems”.
A mixture of presenters from University of Southampton,
Public Health Dorset and Dorset Clinical Commissioning Group (CCG) kept the content varied and representative from across the region.
In December 2020 we facilitated our first remote training session on Data Visualisation, which enabled a smaller cohort to share and discuss best practice agnostic of software – the principles of how to tell a story with data and understand the why, not just report the what.
Dorset Primary Care Network (PCN)
Data Ambassadors and Dorset Integrated Care System (ICS) Intelligence Champions (and friends!) have continued in earnest. Calls rather than face to face meetings have enabled many more participants and facilitated the peer learning and sharing that are
the bedrock of these groups via screen share demonstrations and group discussion.
Along with its many challenges, the emergence of COVID
in March 2020 brought opportunities and highlighted the
urgent need to collate timely system-wide data at speed,
in one place. DiiS became the obvious choice and our
system-wide COVID reporting has received accolades on a
national stage.
Collating all COVID test data, along with all
other COVID-related data metrics across health and care,
presented in an automated live system–wide view of
COVID cases, across all care settings, enables us to better
understand the spread of the disease and its impact on services.
Available to all our partners, this has supported multiple workstreams over the last nine months, including Public Health Dorset’s epidemiology modelling. Throughout the year we have developed analytics focusing on our vulnerable and at-risk populations.
The DiiS tools have helped colleagues across the ICS to identify specific patient groups who may benefit from a directed, pro-active approach. For example, using live mental health data from primary care, we can view our population who have mental health conditions including learning disabilities and serious mental illness holistically.
The data can be stratified and segmented by demographics, socio-economic factors, geography, ethnicity and associated long term physical health conditions.
To support the health inequalities agenda we have been able to use the DiiS to provide interactive and filterable analytical tools with a number of metrics including deprivation, such as most and least 20% deprived, as well as other vulnerabilities including risk of social isolation, unhealthy behaviours and active safeguarding flags.
Using this data in their COVID response, PCN colleagues designed a different intervention for each group using the breadth of workforce available to them including Advanced Nurse Practitioners, Social Prescribers and the voluntary sector.
Somerset Post-COVID-19 Assessment Service https://nhssomerset.nhs.uk/my-health/my-local-health-services/covid-19-recovery-services/
With the winter months fast approaching and the usual bugs and illnesses starting to circulate, it’s a good time to remember that for some people, the impact of COVID-19 lasts longer than just a few days.
In January 2023 the Office for National Statistics estimated that around two million people (3.1% of the population) in the UK were living with Post-COVID-19 Syndrome – around 1 in 30 people in the country.
If Somerset had an average number of cases of people with Post-COVID-19 Syndrome, it could form a town the size of Wellington!
You could have family members or colleagues living with this condition, with some even suffering in silence, concerned they won’t be believed.
People with Post-COVID-19 Syndrome may visit our trust as outpatients, or be admitted with other conditions, and some tell us when they mention their ‘Post-COVID-19 Syndrome’ symptoms, they are not believed or understood.
There are approximately 200 symptoms people can experience, but the most common are:
- 71% Fatigue;
- 52% Difficulty concentrating (Brain Fog);
- 48% Shortness of breath
- 47% Muscle aches.
People also reported the impact it has on their daily life and their ability to work:
- 77% Symptoms adversely affected day to day activities;
- 19% Ability to undertake day to day activities had been ‘limited a lot’.
By reading this article you can help to support people by pointing them in the right direction for help from our Somerset Post-COVID-19 Assessment Service, or simply acknowledging how they are feeling.
The development of our Somerset Post-COVID-19 Assessment Service and how it works
In early 2021 a series of Post-COVID-19 Assessment Services were developed across England as part of the government’s response to the pandemic.
A total of 86 clinics were set up to offer Post-COVID-19 assessment, to identify people who were experiencing Post-COVID-19 Syndrome and to look at what support they needed, as well as providing an onward referral to a service that best meets their needs.
Somerset Post-COVID-19 Assessment Service
..is commissioned by the NHS Somerset Integrated Care Board (ICB) to provide a specialist assessment, diagnosis and rehabilitation for adults aged 18 years or over within Somerset.
The service is for those who are experiencing signs and symptoms that developed during or following a confirmed or suspected COVID-19 infection, which continue for more than 12 weeks. The assessment is based on NICE guidelines and includes a personalised management plan to support recovery.
A referral pathway has been developed between the service and a number of specialist or secondary care services – many of which are run by our NHS trust.
All patients referred to the service get an assessment with one of the Post-COVID-19 Specialist GPs working within the service – these may be via phone, ‘Attend anywhere’, or in person if requested.
As the service has grown, care pathways have become more individualised and tailored to each patient’s needs.
There are now a number of treatment pathways offered by the service, including:
- Fatigue management groups;
- Physio support for breathing pattern disorder;
- Cognitive screening and support;
- Employment advice workshops;
- 1 to 1 clinical input;
- direct access to Talking Therapies.
The management plan given to patients includes advice, support and self-help resources, or a referral to specialist services for support or rehabilitation where appropriate.
After a patient has completed their assessment and management plan, they are discharged from the service back into the care of their GP.
Lorraine Perry, our lead for the service, said she was impressed with the way colleagues went above and beyond to set up a service that was completely new to healthcare.
“In many ways our Post-COVID-19 Assessment Service is a service like no other,” she said. “We have had to set it up and then adapt and develop as we find out more about COVID-19.”
Our colleagues at NHS England (South West) oversaw the setup of clinics within the region, but due to the speed Post-COVID-19 Assessment services were set up across the country, with little evidence about the condition and no national guidance, there is understandably variation within services across England. This inevitably has an impact in the way they are run, and the experience of patients.
Lorraine continues: “Our team has been amazing, as despite the many challenges we have faced, the commitment our colleagues have shown to increase their understanding of this condition, and to provide a service that is responsive both to new evidence and patients’ needs, is at the heart of what we do.
“I cannot thank my colleagues enough for their support and determination in the continued development of this service.
“When the service was set up in December 2020, we only had a single GP and colleague from the former Somerset Clinical Commissioning Group involved. By February 2021, we were able to begin offering 1:1 telephone assessments to patients.
“We now have a service lead, administrator, two GPs with a special interest in Post-COVID-19 Syndrome, two specialist occupational therapists, a physiotherapist, a health psychologist, two specialist fatigue practitioner nurses, two health navigators, and a peer support group facilitator.
“We’re able to provide a more comprehensive self-management group programme, with our health navigators supporting patients to understand the services available to them, and how to access community and voluntary resources when needed.
“Since February 2022, our peer support group facilitator has developed a number of online peer support groups, bringing people who experience Post-COVID-19 Syndrome together, to help reduce the sense of isolation that so many describe, as well as sharing information on the strategies and advice that are supporting them.
“This year we have added ‘Moving Forward with Peer Support’ meetings for those who are starting to navigate returning to work and life, while still progressing on the ‘Post-COVID’ journey – we’re making some great headway.”
Colleagues in our Post COVID-19 Assessment Service have developed a website and leaflets to support clinicians and patients.
This includes information on the how to support patients when they have appointments or admission within the trust.
Rachael Rowe, Head of Long Term Conditions at NHS Somerset says “We know it is vital that people with Long COVID get the support they need. Our Covid Recovery Service enables us to draw on specialist services across Somerset such as mental health and physio support, in a co-ordinated manner to address a patients individual needs, ensuring they can benefit from a wide range of specialist advice and support.”
In recent months a live view of our flu vaccination status is informing the winter flu campaign and communications strategies as well as helping clinicians to target hard to reach populations, and we will shortly be doing the same for COVID vaccinations.
To enhance this offer, we started the year with the ambition to enable clinicians to re-identify cohorts of their patients to support case finding, Multi-Disciplinary Team (MDT) support and other population health management initiatives via our DiiS tools. Whilst this proved to be one of the year’s more challenging tasks, we eventually delivered the first live re-identification tool in the
country.
As the DiiS’ response to the COVID pandemic evolved we started to get noticed by health and care colleagues across the South West region and beyond and were approached by many to explain its evolution. As a result, we are now hosting a national peer learning network, run in collaboration with NHSEI, and with participants from across the country, to share experiences as we mature as intelligence functions within ICS’.
We have contributed Dorset case studies to national guidance on
how to build a successful intelligence function and had an audience with the Director of Emergency Response at NHSE, Professor Keith Willett, no less!
As well as garnering attention across the health and care system, we have also generated interest from industry partners such as Microsoft, who have featured us in their Customer Stories.
We are honoured to have:
- Featured in the Association of Professional Healthcare Analysts
(AphA) magazine; - Headlined at Dorset’s Digital Futures Festival;
- Participated in a global PHM summit;
- Shortlisted for the Institute of Collaborative Working (ICW)
Collaborative Working Awards; - Nominated for the Health Service Journal (HSJ) Healthcare
Excellence Awards; - Nominated for the Skills for Health Our Health Heroes Awards.
